About STIs and what to know before doing you-know-what.


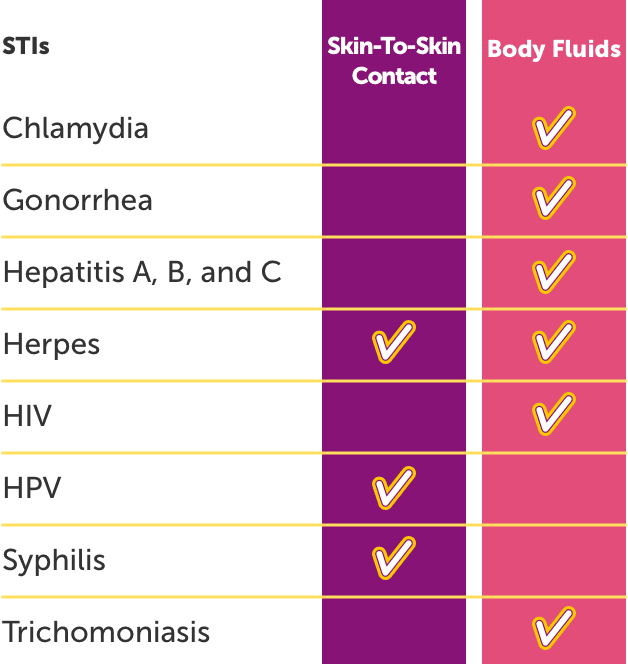
STI stands for “sexually transmitted infection,” which can be spread through skin-to-skin contact and body fluids during oral, vaginal, and anal sex.
Getting busy? Here’s a breakdown of how some STIs are most commonly passed: